Hypercoagulable States
A hypercoagulable state (also called thrombophilia), is a fancy word for a host of different clotting disorders. It means you have a predisposition to excessive blood clotting (aka thrombus formation). Sometimes, we call this “sticky blood” to simplify this constellation of clotting disorders. Any condition that promotes excess clotting or decreases the body’s ability to stop clot formation can lead to a hypercoagulable state. In general, this process involves a complex cascade of events where the blood vessels, platelets, and clotting factors interact to form a clot. Natural blood thinners produced by the body are crucial to help regulate this cascade and prevent excess clotting. If either the clotting cascade or the regulation by natural blood thinners goes awry, a hypercoagulable state can develop.
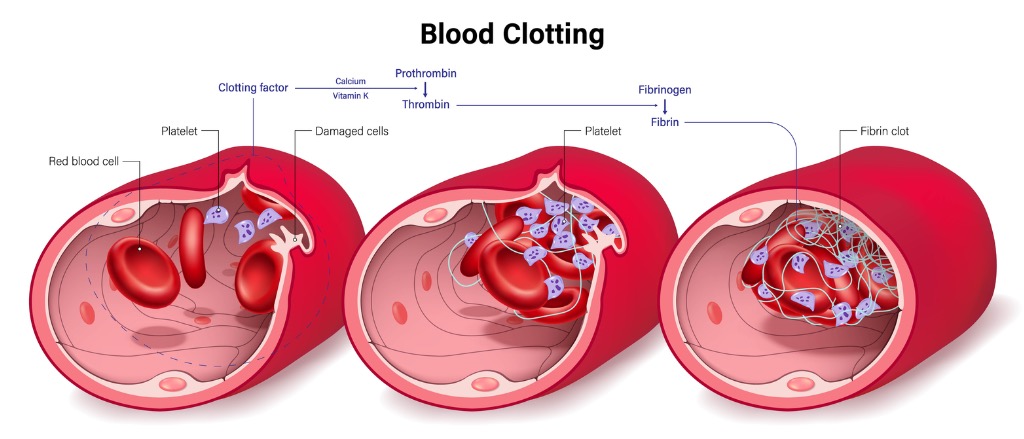
The Basics of Blood Clot Formation
Normally, clotting factors stay inactive in the blood. But when there is an injury to the blood vessel wall, the clotting factors are rapidly activated, which leads to clot formation. A clot is made up of a platelet plug stabilized by fibrin mesh, and it is meant to stop the bleeding from the injured blood vessel in a process called hemostasis.
The body has ways to regulate the clotting process so that clots form only where there’s an injury, and only grow to a size that will stop the bleeding without blocking the blood vessel. Special “clot-blocking” proteins like protein C and protein S work together to inactivate the clotting factors. Another clot-blocking protein called antithrombin III decreases thrombin production and halts the clotting cascade. The body relies on the balance of the clot-forming and clot-blocking agents to ensure that there is enough clotting to stop bleeding but not so much that it causes dangerous clots.
Hypercoagulable States
A hypercoagulable state develops when clotting factors become overactive or clot-blocking proteins are either deficient or malfunctioning. Several different conditions, both inherited (genetic) and acquired, can cause this imbalance and promote excess clotting. Acquired hypercoagulable states are much more common than inherited ones, but testing for an inherited clotting disorder may be indicated for people with certain risk factors, as detailed below.
Inherited Hypercoagulable Disorders
There are many different types of inherited hypercoagulable disorders. We will focus on the more common ones and the ones most frequently tested for when a patient is believed to have one of these disorders.
- Factor V Leiden
- Basics: The most common inherited hypercoagulable disorder. It results from a mutation in the F5 gene that encodes the factor V clotting factor. This mutation makes the clotting factor resistant to the clot-blocking protein called protein C, which increases a person’s risk of blood clots in the veins. People with factor V Leiden are twice as likely as others to form a clot and are at the greatest risk when they have other risk factors for excessive clotting, including pregnancy, hormone replacement therapy, and smoking.
- Testing: Consists of either genetic testing for the factor V Leiden mutation or a blood test for resistance to protein C.
- Treatment: There is no cure for factor V Leiden. The main treatment is blood thinners for those who have suffered a clot. People with the gene mutation but no history of blood clot and who are not pregnant do not need to take blood thinners preventively, but they do need to be aware of their increased risk and watch for signs and symptoms of a blood clot. For pregnant women who are at higher risk (because they have a strong family history, prior blood clot, or recurrent pregnancy loss), taking blood thinners preventively may be recommended.
- Prothrombin gene mutation
- Basics: The second most common inherited hypercoagulable disorder. It results from a “gain of function” mutation in the prothrombin gene that makes it more active in the blood, which leads to increased thrombin levels and clot formation. People with the prothrombin gene mutation are 3-4 times more likely than others to develop blood clots. Like factor V Leiden, this mutation mainly increases the risk of blood clots in the veins, but in certain situations, it can also increase the risk of blood clots in the arteries.
- Testing: Consists of genetic testing for the prothrombin gene mutation.
- Treatment: There is no cure for the prothrombin gene mutation. As with factor V Leiden, the main treatment is blood thinners for patients who have a clot. Nonpregnant individuals who have the mutation, but have not had a blood clot do not merit blood thinners unless there is a clinical indication such as an acute medical illness or recent surgery. For pregnant women who carry the mutation and who are considered high-risk, preventive blood thinners may be recommended.
Protein C/Protein S/Antithrombin Deficiency- Basics: These are three separate inherited hypercoagulable disorders caused by mutations in the protein C, protein S, and antithrombin genes, respectively. All three proteins are natural blood thinners, and when they are deficient or defective, there is an increased risk of thrombosis. These thrombophilias are considered higher-risk because people who have them have 6 to 7 times more risk of venous clot formation than most people. These conditions have also been linked to an increased risk of arterial blood clots.
- Testing: Consists of blood tests to look at protein C levels/activity, protein S levels/activity, and antithrombin activity. Notably, blood thinners can make these tests less accurate, so blood thinners are usually stopped before testing unless stopping them is considered too risky.
- Treatment: There is no cure for these deficiencies. Blood thinners are the main treatment, although in people with protein C and protein S deficiency, warfarin must be used cautiously because it can cause skin necrosis. In high-risk individuals with no history of blood clots, preventive blood thinners may be recommended. Similarly, blood thinners may be used preventively during pregnancy or before surgery in certain individuals. For individuals with one of these mutations, it is recommended to avoid other clot-promoting substances such as tobacco, and medications containing estrogen.
-
Who Should be Screened for an Inherited Hypercoagulable Disorder?
Not all patients who suffer from a blood clot need to be screened for an inherited hypercoagulable disorder. Testing is usually recommended if:
- The blood clot occurs in a young individual (<50 years) without any identifiable cause
- There is a strong family history of blood clots
- There is a family history of a hypercoagulable disorder
- The blood clot occurs in an unusual location (like a portal vein or a cerebral vein)
- The person suffers a second blood clot
- The person develops warfarin-induced skin necrosis (if that happens, testing for protein C and protein S deficiencies may be indicated)
Acquired Hypercoagulable Disorders
Acquired hypercoagulable disorders are much more common than inherited ones. The more common causes of acquired hypercoagulable states include:
- Medications
- Estrogen-containing medications like oral contraceptives and hormone replacement therapy have been shown to increase the risk of clotting and stroke
- Cancer treatments like tamoxifen, certain chemotherapies, and immunotherapies also increase the risk of clotting
- Antifibrinolytic medications, which are usually given to patients with severe injuries to promote clotting
- Pregnancy
- Associated with an increase in clotting factors and a decrease in clot-blocking proteins like protein C and protein S, which causes a hypercoagulable state
- Smoking
- The chemicals in tobacco products make platelets more prone to clumping and clotting
- Cancer
- Cancers of the pancreas, lung, stomach, colon/rectum, and kidney, as well as multiple myeloma, result in the highest risk of blood clots
- Patients with more advanced stages and grades of cancer, as well as patients with metastatic cancer, have a greater risk of blood clots
- Immobility or Recent Illness, Surgery, or Hospitalization
- Periods of immobility lead to venous stasis, where the blood does not move as easily through the circulatory system. Blood that isn’t moving is more likely to clot.
- Autoimmune conditions
- Antiphospholipid syndrome (APS) is an autoimmune condition that is strongly associated with an increased risk of venous and arterial blood clots. It can arise in otherwise healthy people and in people with another autoimmune condition, like lupus. In people with APS, the antiphospholipid antibodies attack normal blood proteins, causing platelets to clump together and activate the clotting cascade. APS has been associated with several serious conditions, including recurrent pregnancy loss, stroke, and blood clots in the legs and lungs. For patients who might have APS, there is a blood test that looks for antiphospholipid antibodies. If the test is positive, the patient often will be treated with warfarin and aspirin for the rest of their lives.
- Several other autoimmune conditions also increase the risk of clotting by causing a proinflammatory state
What are the Signs of a Blood Clot? And When Do I Seek Treatment?
One of the most common places where blood clots cause problems is the lower leg. A blood clot there is called a deep vein thrombosis (DVT). Symptoms usually include swelling, tenderness, and redness in the leg. Blood clots in the legs can be dangerous because they can travel to the lungs and cause a pulmonary embolism (PE). A PE can make a person get short of breath easily and can lead to chest pain. If you have any of these symptoms, you need to seek immediate medical attention to ensure you get the right testing and treatment.
If you have a history of clots, a strong family history of blood clots, or a family history of a heritable hypercoagulable condition, or you have suffered from recurrent pregnancy loss, ask your doctor if further testing or treatment is needed.
What Can I Do to Prevent Blood Clots?
There is a lot that a person can do to decrease their risk of forming a blood clot. Healthy diet, regular exercise, and avoiding smoking and alcohol all promote healthy veins and arteries. If you are flying or driving long distances, make sure you take time to walk every two hours to prevent blood from pooling in your legs, as stagnant blood is more likely to clot. In addition, compression socks may be helpful for long journeys as they improve blood flow from the leg veins back to the heart. Conditions that increase your risk of clotting, like surgery or immobility, may call for preventive doses of blood thinners until you are up and moving again as guided by your doctor. If you require medication that can increase your risk of blood clots, or if you have an autoimmune condition or cancer that increases your risk of clotting, make sure you take extra measures to protect yourself, such as remaining active and avoiding smoking. Your physician can also help guide you if you have questions about your risk of clotting so do not hesitate to ask, as they are there to help.
-
Author: Heather Pemberton, MD and Keri Sprung
Editor: Steve Palmer, PhD. ELS
